EAR AND VERTIGO TREATMENT
CONDITIONS & TREATMENT
Ear problems are rampant today – be it infection, hearing loss, blocked ears, discharge from ears or other problems. And age is no bar. Infants as young as one month old or the elderly as old as 90 years can all fall prey to ear problems.
Book Appointment
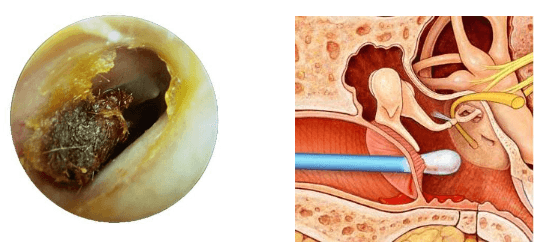
Good intentions to keep ears clean may be risking the ability to hear. The ear is a delicate and intricate area, including the skin of the ear canal and the eardrum. Therefore, special care should be given to this part of the body. Start by discontinuing the use of cotton-tipped applicators and the habit of probing the ears.
Cerumen or earwax is healthy in normal amounts and serves as a self-cleaning agent with protective, lubricating, and antibacterial properties. The absence of earwax may result in dry, itchy ears. Most of the time the ear canals are self-cleaning; that is, there is a slow and orderly migration of earwax and skin cells from the eardrum to the ear opening. Old earwax is constantly being transported, assisted by chewing and jaw motion, from the ear canal to the ear opening where it usually dries, flakes, and falls out.
Earwax is not formed in the deep part of the ear canal near the eardrum, but in the outer one-third of the ear canal. So when a patient has wax blockage against the eardrum, it is often because he has been probing the ear with such things as cotton-tipped applicators, bobby pins, or twisted napkin corners. These objects only push the wax in deeper.
The ears should be cleaned when enough earwax accumulates to cause symptoms or to prevent a needed assessment of the ear by your doctor. This condition is call cerumen impaction, and may cause one or more of the following symptoms:
- Earache, fullness in the ear, or a sensation that ear is plugged
- Partial hearing loss, which may be progressive
- Tinnitus, ringing, or noises in the ear
- Itching, odor, or discharge
- Coughing
Irrigation or ear syringing is commonly used for cleaning and can be performed by a physician or at home using a commercially available irrigation kit. Common solutions used for syringing include water and saline, which should be warmed to body temperature to prevent dizziness. Ear syringing is most effective when water, saline, or wax dissolving drops are put in the ear canal 15 to 30 minutes before treatment. Caution is advised to avoid having your ears irrigated if you have diabetes, a perforated eardrum, tube in the eardrum, or a weakened immune system.
Manual removal of earwax is also effective. This is most often performed by an otolaryngologist using suction, special miniature instruments, and a microscope to magnify the ear canal. Manual removal is preferred if your ear canal is narrow, the eardrum has a perforation or tube, other methods have failed, or if you have diabetes or a weakened immune system.
Wax blockage is one of the most common causes of hearing loss. This is often caused by attempts to clean the ear with cotton swabs. Most cleaning attempts merely push the wax deeper into the ear canal, causing a blockage.
If you are prone to repeated wax impaction or use hearing aids, consider seeing your doctor every 6 to 12 months for a checkup and routine preventive cleaning.
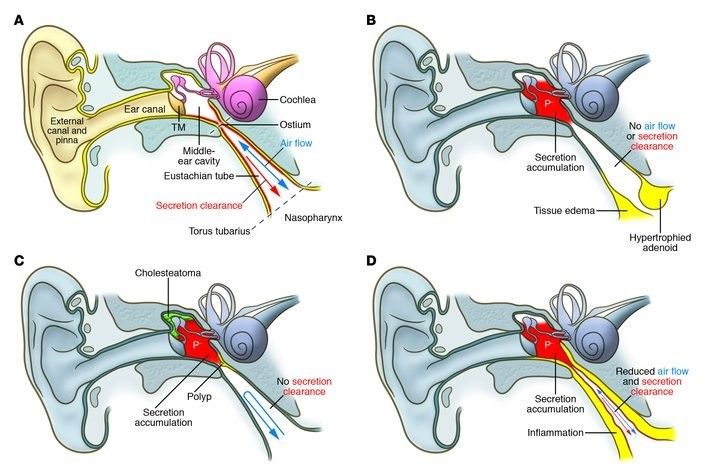
Acute Otitis media is an inflammation of the middle ear (the cavity between the eardrum and the inner ear). Children are more commonly affected than adults because of the small size and horizontal position of their eustachian tube (the passage that connects the back of the nose to the middle ear). The eustachian tubes equalize the pressure between the middle ear cavity and the outside atmosphere and allow fluid and mucus to drain out of the middle ear cavity. This tube may become blocked by a bacterial or viral infection of the upper respiratory tract or by enlarged adenoids. Fluid produced by the inflammation cannot drain off through the tube and instead collects in the middle ear.
Symptoms of Otitis Media
Acute otitis media causes sudden, severe earache, deafness, and tinnitus (ringing or buzzing in the ear), sense of fullness in the ear, irritability, tugging or rubbing the ear, an unwillingness to lie down, fever, headache, a change in appetite or sleeping patterns, fluid leaking from the ear, nausea and difficulty in hearing. Occasionally, the eardrum can burst, which causes a discharge of pus and relief of pain. Complications of a single episode of otitis media are rare and include otitis externa (inflammation of the outer ear), and spread inward from the ear to the skull, causing, mastoiditis (inflammation of the mastoid bone cells), or into the brain, causing meningitis (inflammation of the membranes covering the brain and spinal cord) or a brain abscess. Complications in recurrent otitis media include perforation of the ear drum, damage to the bones in the middle ear (sometimes causing total deafness) or a cholesteatoma (a matted ball of skin debris which can erode bone and cause further damage to the ear).
Diagnosis of Otitis Media
Otitis media can be detected by examining the ear with an otoscope. In addition, two tests may be performed to give the E.N.T. Specialist information that cannot be learned through observation only. One of these tests is an audiogram, in which tones are sounded at various pitches. An audiogram is used to measure how much hearing loss has occurred. The second test, called a tympanogram, measures the air pressure in the middle ear; this indicates how well the eustachian tube is functioning.
Treatment of Otitis Media
After the diagnosis is made, a conservative treatment plan is considered by your otolaryngologist, considering the patient’s age, risk factors for having resistant bacteria, immunization status, and hearing status.
Surgery
Your doctor may recommend surgery if the child’s infection fails to respond to antibiotics, if the ear infections are chronic or hearing loss is indicated.
THE OPTIONS INCLUDE
Adenoidectomy. The doctor may suggest removing the adenoids (adenoidectomy). This procedure is only recommended for children 4 years of age or older, if the otitis media has lasted three months or more and the adenoids are repeatedly inflamed. Tonsillectomy. The doctor may suggest removing the tonsils (tonsillectomy) along with Adenoidectomy. This procedure is only recommended for children 4 years of age or older, if the otitis media has lasted three months or more and the tonsils are repeatedly inflamed. If there is damage to the eardrum the doctor may suggest tympanoplasty (surgical closure of a perforation in the eardrum by means of a tissue graft).
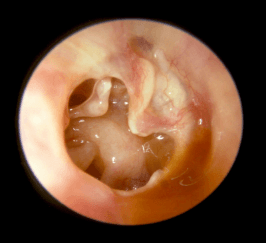
Chronic suppurative otitis media (CSOM) is a chronic inflammation of the middle ear and mastoid cavity. Clinical features are recurrent ear discharge through a tympanic perforation, with hearing loss of varying severity.
The tympanic membrane is perforated in CSOM. If this is a tubotympanic perforation, it is usually ‘safe’, whilst atticoantral perforation is often ‘unsafe’. Safe or unsafe depends on the presence of cholesteatoma:
- Safe CSOM is CSOM without cholesteatoma. It can be subdivided into active or inactive depending on whether or not infection is present.
- Unsafe CSOM involves cholesteatoma. Cholesteatoma is a non-malignant but destructive lesion of the skull base.
- Multiple episodes of acute otitis media (AOM).
- Living in crowded conditions.
- Being a member of a large family.
- Attending daycare.
- Socioeconomic status.
- Craniofacial anomalies increase risk: cleft lip or palate, Down’s syndrome, cri du chat syndrome, choanal atresia, and microcephaly all increase the risk of CSOM.
- CSOM presents with a chronically draining ear (>2 weeks), with a possible history of recurrent AOM, traumatic perforation, or insertion of grommets.
- The otorrhea should occur without otalgia or fever.
- Fever, vertigo and otalgia should prompt urgent referral to exclude intratemporal or intracranial complications.
- Hearing loss is common in the affected ear. Mixed hearing loss (conductive and sensorineural) suggests extensive disease.
- The external auditory canal may possibly be oedematous but is not usually tender.
- The discharge varies from fetid, purulent and cheese-like to clear and serous.
- Granulation tissue is often seen in the medial canal or middle ear space.
- The middle ear mucosa seen through the perforation may be oedematous or even polypoid, pale, or erythematous.
- An audiogram will normally show conductive hearing loss. Mixed hearing loss may suggest more extensive disease and possible complications.
- X-ray Mastoids lateral oblique view.
- A fine-cut CT scan can reveal bone erosion from cholesteatoma, ossicular erosion, involvement of petrous apex and subperiosteal abscess.
- MRI is better if intratemporal or intracranial complications are suspected
- Conservative treatment of CSOM consists of 3 components:
- An appropriate antibiotic
- Regular intensive aural toilet to remove debris
- Control of granulation tissue
- In safe inactive CSOM, once infection has been controlled, a tympanoplasty is usual to prevent recurrent infection.
- Surgery is required in unsafe CSOM, as cholesteatoma can cause serious and possibly fatal complications. Classical radical mastoidectomy, modified radical mastoidectomy or the ‘combined approach tympanoplasty’ may be used depending on the extent of cholesteatoma and, more importantly, the experience of the surgeon. Whatever the procedure chosen, the aim of surgery is to remove all disease and to give the patient a dry and functioning ear.
- Facial paralysis can occur with or without cholesteatoma. Surgical exploration with mastoidectomy should be undertaken promptly.
- Where conductive hearing loss has resulted from CSOM (due to perforation of the tympanic membrane and/or disruption in the ossicular chain), surgical removal of the infection and cholesteatoma, followed by ossicular chain reconstruction, will reduce hearing loss.
- Complications of CSOM are rare but potentially life-threatening. Intratemporal complications include:
- Petrositis
- Facial paralysis
- Labyrinthitis Intracranial complications include:
- Lateral sinus thrombophlebitis
- Meningitis
- Intracranial abscess Sequelae include:
- Hearing loss
- Tympanosclerosis
- There is a good chance of control of infection.
- The recovery of hearing loss varies, depending on the cause. Conductive hearing loss often can be partially corrected with surgery.
Risk factors
Symptoms
Signs
Investigations
Management
Surgical
Complications
Prognosis
A glue ear develops when phlegm and mucus from the nose pass up the thin Eustachian tube into the middle ear. It is difficult for these thick, sticky secretions to escape through the Eustachian tube to the back of the nose, particularly if the adenoids which surround the opening of the tube in to the nose are swollen.
There is a feeling of blockage in the affected ear similar to that felt when descending (more common) or ascending a mountain. Glue may also be responsible for a middle ear infection (Otitis media) and deafness.
Examination of the ear by an otoscope (magnifier and light) shows an opaque and bulging ear drum and special instruments can measure the pressure in the middle ear. The surgical insertion of a small tube (grommet) through the ear drum to relieve the pressure is often necessary. Recurrent cases may require the surgical removal of the adenoids, which are lymph nodes surrounding the nasal opening into the Eustachian tube, There are very good results after appropriate treatment, but the problem may recur after the grommets fall out.
Affecting the outer ear, swimmer’s ear is a painful condition resulting from inflammation, irritation, or infection. These symptoms often occur after water gets trapped in your ear, with subsequent spread of bacteria or fungal organisms. Because this condition commonly affects swimmers, it is known as swimmer’s ear. Swimmer’s ear (also called acute otitis externa) often affects children and teenagers, but can also affect those with eczema (a condition that causes the skin to itch), or excess earwax. A common source of the infection is increased moisture trapped in the ear canal, from baths, showers, swimming, or moist environments. When water is trapped in the ear canal, bacteria that normally inhabit the skin and ear canal multiply, causing infection of the ear canal.
The most common symptoms of swimmer’s ear are itching inside the ear and pain that gets worse when you tug on the auricle (outer ear). Other signs and symptoms include fever, discharge, swollen lymph nodes. Swimmer’s ear needs to be treated to reduce pain and eliminate any effect it may have on your hearing, as well as to prevent the spread of infection
If left untreated, complications resulting from swimmer’s ear may include:
Hearing loss. When the infection clears up, hearing usually returns to normal.
Recurring ear infections (chronic otitis externa). Without treatment, infection can continue.
Bone and cartilage damage (malignant otitis externa). Ear infections when not treated can spread to the base of your skull, brain, or cranial nerves. Diabetics and older adults are at higher risk for such dangerous complications.
Treatment for the early stages of swimmer’s ear includes careful cleaning of the ear canal by your otolaryngologist and use of eardrops that inhibit bacterial or fungal growth and reduce inflammation.
Otosclerosis is a condition of the middle ear and mainly affects the tiny stapes bone. It causes gradual hearing loss. The term otosclerosis is derived from the Greek words for “hard” (scler-o) and “ear” (oto). It describes a condition of abnormal growth in the tiny bones of the middle ear, which leads to a fixation of the stapes bone. The stapes bone must move freely for the ear to work properly and hear well.
The ear is divided into three parts – the outer (external) ear, the middle ear, and the inner ear. The middle ear behind the eardrum is filled with air. Air comes from the back of the nose up a thin channel called the Eustachian tube. In the middle ear there are three tiny bones (ossicles) – the malleus, incus and stapes (also known as the hammer, anvil and stirrup). The inner ear includes the cochlea and semicircular canals.Sound waves come into the outer (external) ear and hit the eardrum. The sound waves cause the eardrum to vibrate. The sound vibrations pass from the eardrum to the middle ear bones. The bones then transmit the vibrations to the cochlea in the inner ear. The cochlea converts the vibrations to sound signals which are sent down a nerve from the ear to the brain, allowing us to hear.
Otosclerosis is a condition that mainly affects the stapes, one of the tiny bony ossicles in the middle ear. What happens in otosclerosis is that abnormal bone material grows around the stapes.The abnormal bone reduces the movement of the stapes, which reduces the amount of sound that is transferred to the cochlea. The growth of the abnormal bone is very gradual. The hearing loss is known as conductive hearing loss. It usually first develops between the ages of 15 and 35 but sometimes develops in younger children. Women are affected twice as often as men. Pregnancy is not a cause but may make the condition worse, so symptoms are commonly first noticed during pregnancy.
You will need to be seen by an ear, nose and throat specialist to diagnose otosclerosis. Hearing tests will show a specific pattern of hearing loss in otosclerosis. The specialist may also use a small device that is placed in your ear, called a tympanometer. This can help them look at the movement of the bones within your ear. In otosclerosis, the stapes will move less. This test is very quick and does not cause any pain. If the hearing loss is mild, the otolaryngologist may suggest continued observation and a hearing aid to amplify the sound reaching the ear drum. Sodium fluoride has been found to slow the progression of the disease and may also be prescribed. In most cases of otosclerosis, a surgical procedure called stapedectomy is the most effective method of restoring or improving hearing.
A persistent, high pitched ringing, swooshing or other type of noise that seems to originate in the ear or head is called tinnitus. It is a very annoying symptom, as the noise may continue day and night without relief and drown out quieter noises that the person is trying to hear. In most cases tinnitus is not a serious problem and can be treated or in time will simply go away.
Tinnitus is not a disease but a symptom of an underlying condition. One of the most common conditions associated with tinnitus is presbyacusis (hearing loss with age). Tinnitus is also associated with conditions such as wax in the outer ear canal, middle ear infections, otosclerosis (fixation of the middle ear bone), Meniere’s syndrome ( a problem affecting both hearing and balance) and acoustic neuroma ( a small, rare tumor of the acoustic nerve). If head noises persist, particularly if they are on one side or are associated with loss of hearing or dizziness, medical attention is recommended.
Rare causes include persistent high blood pressure, some neuroses (eg. schizophrenia), altitude sickness (ascending rapidly to heights over 3000m), Costen syndrome (abnormal stresses are placed on the jaw joint and muscles of chewing) and Cogan syndrome. Excess caffeine from coffee, cola drinks or medications (e.g. Stimulants) can cause tinnitus as a side effect as may excess aspirin and some malaria medications (e.g. quinine). The cause is a build-up in the pressure of the fluid inside the hearing and balance mechanisms of the inner ear.
A full description of your symptoms can help your doctor determine the probable cause of your tinnitus. Your doctor will want to know if the noise is in one ear or both, how long you’ve had tinnitus, if you have trouble hearing or are prone to losing your balance.
Tinnitus is not a disease but a symptom and can be caused by numerous conditions. To find out what may be causing your problem, a complete ENT examination and special tests may be necessary. The key to successful treatment of tinnitus is getting the most accurate diagnosis possible.
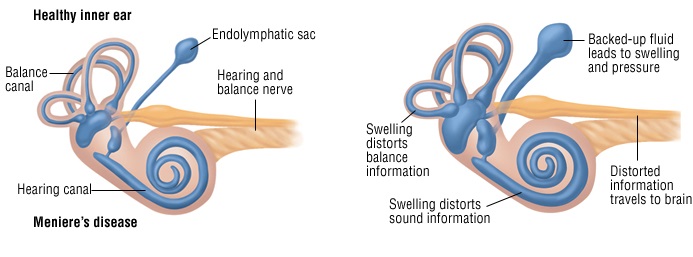
Meniere’s disease is a vestibular disorder usually presenting in adults 30 to 50 years of age. The classic syptoms are episodic vertigo, low-pitched tinnitus, fluctuating low-frequency sensorineural hearing loss (SNHL) and a feeling of fullness in the affected ear. The vertigo is intense for 1 to 2 hours, followed by unsteadiness for a few days. The hearing loss and tinnitus usually resolve after an attack but may increase with each episode and the vertigo may persist. Drop attacks (“crisis of Tumarkin”), during which the patient loses extensor tension and falls to the ground fully conscious, may occur late in the disease. The causes of Meniere’s disease is unknown, but autoimmunity, endocrine disorder and disturbed labyrinthine electrolyte balance are suspected. The diagnosis is made by the history because the physical examination is normal except during an attack. Audiometry shows low-frequency SNHL and ENG shows hypoactivity on the effected side.
You should consult an otolaryngologist who will ask questions about your symptoms and ask you to describe what happens when you have an attack. Some tests might include hearing and blood tests, an MRI or CT scan, or special tests that check your balance and how well your ears work.
The treatment begins with eating a low-salt diet, avoiding tobacco and caffeine and taking diuretic. Vestibular suppressants are needed only during an acute attack. If medical treatment fails, surgery (e.g., endolymphatic shunt, vestibular nerve section, labyrinthectomy) may help. Chemical destruction of the vestibular system with transtympanic aminoglycosides has succeeded in controlling vertigo in some patients.
Meniere’s disease is often frustrating for people who have it. You may have to change the way you live to control the attacks. You should follow your doctor’s advice about your diet, and about cutting out alcohol, caffeine and smoking. Since stress may cause an attack, you may have to find ways to limit the stress in your life or learn how to deal with stress more effectively. Let your family, friends and co-workers know about the disease. Tell them how they can help you if you have an attack.
Dizziness, Balance & Motion Sickness
Each year more than two million people visit a doctor for dizziness, and an untold number suffer from motion sickness, which is the most common medical problem associated with travel. Remember: Most cases of dizziness and motion sickness are mild and self-treatable disorders. But, severe cases and those that become progressively worse, deserve the attention of a physician with specialized skills in diseases of the ear, nose, throat, equilibrium, and neurological systems. The underlying cause of symptoms may include allergic or metabolic disturbances, trauma, inner ear fluid fistulas, a viral infection called vestibular neuritis involving the inner ear nerve, interference with the circulation of blood to the inner ear that is sudden and intermittent in character, small particles of calcium in the semicircular canals. Less common causes of dizziness may include autoimmune inner ear disease (AIED), acoustic tumors (known as acoustic neuromas or vestibular nerve schwannomas), Meniere’s disease, cochlear hydrops and complete loss of vestibular function due to toxic effects of some diseases or
What is dizziness?
Some people describe a balance problem by saying they feel dizzy, lightheaded, unsteady, or giddy. This feeling of imbalance or disequilibrium, without a sensation of spinning, is sometimes due to an inner ear problem.
What is vertigo?
A few people describe their balance problem by using the word vertigo, which comes from the Latin verb “to turn”. They often say that they or their surroundings are turning or spinning. Vertigo is frequently due to an inner ear problem.
What is motion sickness and sea sickness?
Some people experience nausea and even vomiting when riding in an aeroplane, automobile, or amusement park ride, and this is called motion sickness. Many people experience motion sickness when riding on a boat or ship, and this is called seasickness even though it is the same disorder. Motion sickness or seasickness is usually just a minor annoyance and does not signify any serious medical illness, but some travellers are incapacitated by it, and a few even suffer symptoms for a few days after the trip.
Treatment:
In most cases medical (prescribed medicines) treatment is helpful in eliminating the symptoms of vertigo, dizziness and motion sickness and surgery is seldom necessary. Some medicines used to treat balance disorders include diuretics and vasodilators (blood vessel dilators like niacin), and physicians may also recommend allergy treatment and diet regulation to reduce episodes of vertigo.
Facts about newborn hearing loss:
Hearing loss is the most frequently occurring birth defect, occurring more frequently than all metabolic disorders screened for at birth combined. Approximately 3 in 1000 babies are born with a mild hearing loss or greater. 1 in 1000 babies are born deaf, and 90% of children with hearing loss are born to normal-hearing parents. Over 50% of babies born with hearing loss have no known risk factors for hearing loss. A hearing screening can be completed in as little as 5 minutes. Even a mild hearing loss can significantly impact a child’s ability to learn speech & language. Children identified with hearing loss and receiving early intervention services prior to 6 months of age achieve significantly higher language scores than children identified after 6 months of age.
Hearing & Speech Milestones:
-
Newborn (Birth to 6 Months)
- Does not startle, move, cry or react in any way to unexpected loud noises.
- Does not awaken to loud noises.
- Does not freely imitate sound.
- Cannot be soothed by voice alone.
- Does not turn his/her head in the direction of your voice. Young infant (6 months to 12 months)
- Does not point to familiar persons or objects when asked.
- Does not babble, or babbling has stopped.
- By 12 months does not understand simple phrases by listening alone, such as “wave bye-bye,” or “clap hands.” Infant (3 months to 2 years)
- Does not accurately turn in the direction of a soft voice on the first call.
- Is not alert to environmental sounds.
- Does not respond on the first call.
- Does not respond to sounds or does not locate where the sound is coming from.
- Does not begin to imitate and use simple words for familiar people and things around the home.
- Does not sound like or use speech like other children of similar age.
- Does not listen to TV at a normal volume.
- Does not show consistent growth in the understanding and the use of words.